CC: CP - the PE
Ok, so you have a pt with no obvious cause for CP, what do you examine and why? Let’s say you have a known cause for CP, do you need to examine anything?
In a word, YES! Of course, you have to do a physical exam (PE)!!! It can offer SOME useful information.
The problem is…
You’re doing the physical exam wrong!!
Stop doing a head-to-toe PE, and definitely stop documenting a standard normal exam that you didn’t do!
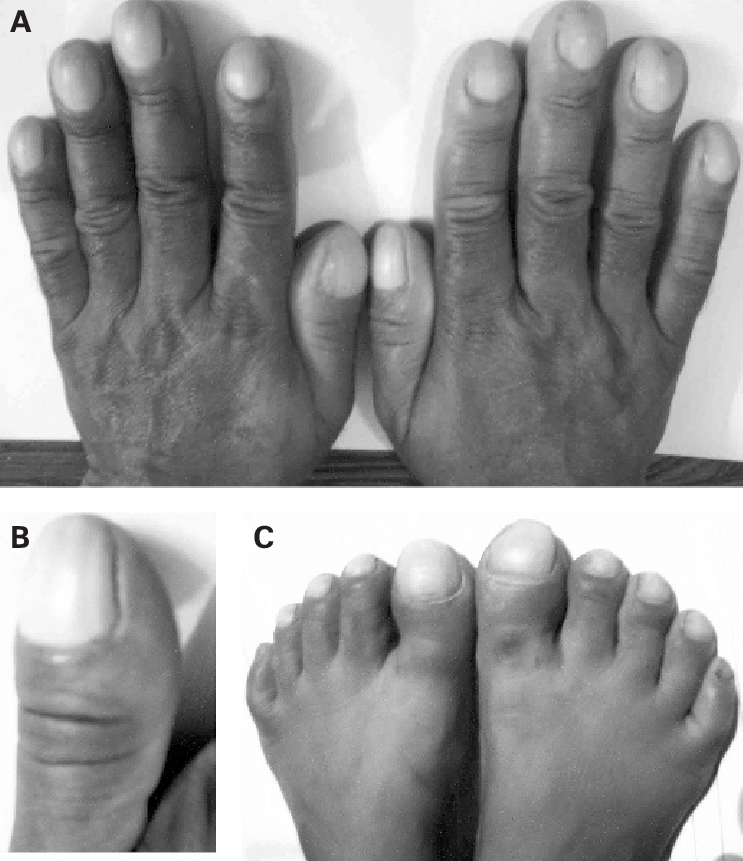
Those changes are congenital, Dr. House!
Do you even know what clubbing is? Stop documenting this finding that is either genetic or took decades to occur due to chronic hypoxia. It’s probably not causing CP. Instead, look at the extremities to assess perfusion (cyanosis, cap refill) and for edema that could be part of new heart failure.
You’re a smart clinician (because you’re reading this post), don’t waste your time looking/listening for things that aren’t pertinent, just to make it look like you know what you’re doing. Go down you’re differential diagnosis and look/listen/feel for them!!!
Look at the skin for herpes zoster, abscess, cellulitis. I’ve seen it before on a dementia patient who didn’t need a “CP work-up” for a painful zoster on her chest.
Actually, look at the neck for JVD of heart failure.
The abdomen lies fairly close to the chest and I have been guilty of overlooking acute cholecystitis or other intra-abdominal pathology a time or two only to go back and examine the abdomen and test for a Murphy’s sign.
Don’t miss… A Pneumothorax
Don’t rely on just your stethoscope (and percussion?) to detect a pneumothorax, and DEFINITELY don’t wait for chest x-ray to detect a tension pneumothorax!!!
This patient is dying while waiting for a chest x-ray to be taken!
If only there was a quick, reliable method of detecting pneumothorax at the bedside…oh wait, there is.
Evidence:
Conclusion: The present meta-analysis showed that the diagnostic accuracy of CUS was higher than supine CXR for detection of pneumothorax. It seems that CUS is superior to CXR in detection of pneumothorax, even after adjusting for possible sources of heterogeneity.
Conclusion: The diagnosis of pneumothorax using ultrasound is accurate and reliable; additionally, it can result in timely diagnoses specifically in neonatal pneumothorax. Using this method facilitates the therapy process; lack of ionizing radiation and easy operation are benefits of this imaging technique.
…a few physical exam findings and the clues they may give us to an underlying disease.
Heart sounds - listen for a rub of pericarditis, muffled sounds of pericardial effusion, a new murmur of a valve rupture or regurgitation
Jugular venous distention - might indicate right heart backup in pulmonary embolism, cardiac tamponade or acute heart failure
Lungs sounds - listen for lack of breath sounds in pneumothorax and adventitious sounds like crackles in CHF or rhonchi in pneumonia
Pulses in all 4 extremities - a pulse deficit in any extremity could indicate an aortic dissection
Neuro deficit could also scream dissection (of the carotids) in the context of tearing chest pain.
(gif of JVD)
Use your stethoscope as a “test” to increase or decrease the likelihood of certain diseases.
Thinking of CHF? Start at the bases and listen for rales.
Focal rhonchi occurs in lobar pneumonia so spend the time listening to every lobe if that’s on your differential.
If you think pneumothorax, just go right to POCUS (my opinion), or listen specifically for decreased breath sounds.
Do you know how many times I’ve see RRR in a pt with a-fib? Or no murmurs on a pt with aortic stenosis? It’s better to chart nothing. Instead, auscultate for specific findings pertinent to a differential Dx of CP.
What might that be, you ask?
Systolic ejection murmur heard best at the base of a pt with no know history of aortic stenosis or a loud AS murmur in a pt whom you’re concerned now has critical stenosis causing heart strain.
Aortic insufficiency would sound like a diastolic murmur in the context of a widened pulse pressure you already found.
Listen carefully over the mitral and tricuspid valves susceptible to vegetation in endocarditis.
Listen for that pericardial rub of pericarditis? Yeah right. Muffled heart sounds??? Just grab the ultrasound and look for a pericardial effusion.
Finally, if you have a pt who goes into flash pulmonary edema after an MI, check for a systolic murmur at the apex from acute mitral regurgitation from papillary muscle infarction.
If you didn’t follow any of that, consider retiring your stethoscope or at least relearning how to use it. Despite being a nearly outdated tool, it can offer some specific information.
Let’s recap…
The PE is a useful part of the evaluation of a pt with undifferentiated CP.
Don’t go through the motions of a PE. Take that time to assess for actual diseases.
The list of pertinent disease that can present as undifferntiated CP include the following:
Herpes Zoster or other skin pathology
Pneumothorax - heaven forbid you wait until you get a CXR to consider this!
Pneumonia that in retrospect was fairly obvious but your brain was only thinking cardiac causes of CP
Endocarditis with valvular involvement that could be very important to investigate in a patient that was not forthcoming with an IVDU history.
New CHF from…
Critical aortic stenosis
Aortic insufficiency
Mitral regurgitation
Can you think of more diagnoses to add? I’d love to hear from you.