CC: CP - other important Dx to Document
Other stuff that causes chest pain...
So there you have it. Don't walk into or out of a room with a patient with chest pain without thinking of MI, massive PE, pneumothorax, and dissection.
Next up, all of the other dangerous and not-so-dangerous causes. To name a few...
Pericarditis/myocarditis
Pneumonia/pneumonitis
Esophageal rupture - Boehaaves syndrome
Esophageal spasm
GERD
Incarcerated diaphragmatic hernia (huh? Yeah, that's a thing)
Costochondritis aka Tietz syndrome
Pyelonephritis (I've never seen this)
Herpes zoster (obvious once rash shows up)
Idiopathic (we’ll never know)
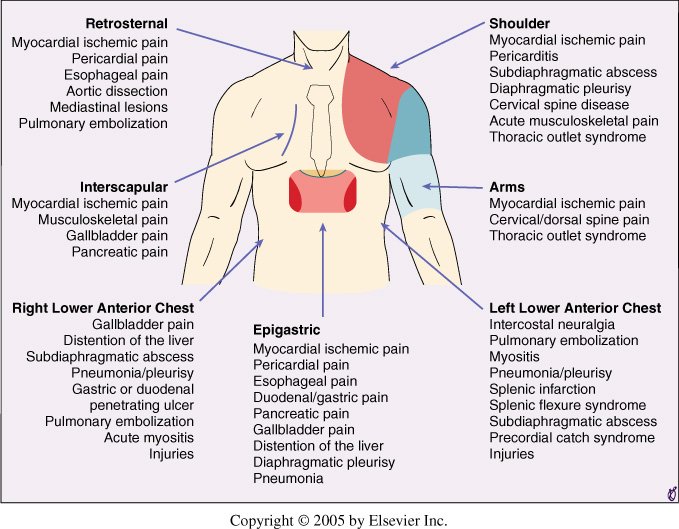
Lists like the one above, and attempting to diagnose based on location and radiation is a waste of time. I highly doubt any trained clinician is going to miss a ruptured esophagus!!! A good history and examination will usually elucidate a non-intrathoracic cause of chest pain. For example,
If a patient is complaining of CP and vomiting blood, think Mallory-Weiss tears, or
If there is a dermatomal rash on the chest, think of shingles, or
If the chest is tender, it could be costochondritis.
The list of causes for (non-obvious) undifferentiated CP is long and can include the following:
Angina (without infarction)
Endocarditis
Acute chest syndrome (in sickle cell patient)
Sub-massive PE
Pericarditis
Pneumonia
Aspiration pneumonitis
Pancreatitis
GERD
Very rare causes
Mediastinitis
Perforated peptic ulcer
Spontaneous coronary artery dissection
Stress (takotsubo) cardiomyopathy
It is hard to say what from the list above should be routinely included in your MDM, but here is what I have come up with (for now)…
Infectious etiology considered. History and lung exam do *** support pneumonia or respiratory infection. Patient is not at risk for aspiration pneumonia. There is *** history of recent IVDU and *** signs or septic emboli on examination to suggest endocarditis.
Gastritis, GERD, and pancreatitis were considered with *** risk factors or historical clues to support this.
Pain is *** increased with lying or relieved with sitting up to suggest pericarditis with *** pericardial effusion seen on bedside ultrasound.
Clinically significant PE was also considered with the patient having *** risk factors. Well's criteria was used to risk stratify with the patient *** for PE. The PERC criteria was *** applied. Further work-up *** indicated.
What about anxiety and chest pain?
Well, it turns out a lot of people in the ED with chest pain (CP) have anxiety about it. That seems to make sense because the reason they came to the ED was because they were worried about the CP. Many people will actually ask me, “Do you think that this pain could be because of my anxiety (or stress)?” Usually, my response is something along the lines of “I wish I had a test for that.”
Anxiety and other emotions can cause many symptoms and physiologic changes (see my Takotsubo syndrome case report). In addition, this study, no surprise, found that about 50% of low-risk CP patients presented during a time of high anxiety. Furthermore, many of these types of patients end up re-presented at a later time. Now, I think it is silly and foolish to make a diagnosis of anxiety “causing CP,” but that does not mean that it isn’t work talking to the patients about their anxiety. At minimum, this might put the patient’s mind at ease (perhaps decrease anxiety), and it may decrease repeat visits. When I do this I generally share the statistics for the HEART score or even show them the calculator and their risk of 30 day adverse outcome. Again, I don’t label CP as “cause by anxiety" but that anxiety can be a strong component of presenting symptoms.
Should you document a discussion about anxiety with patients with no apparent cause for CP?
I don’t think that you will find a consensus opinion, but I would love to hear your thoughts. Personally, I often talk to patients about anxiety when there is no cause found for their CP, but it depends mostly on the state of the patient and if think that they would be open to a discussion. A line I have often told patient’s is that I always take a complaint of chest pain seriously and don’t consider anxiety alone as the cause until I have considered dangerous diagnoses. Sometimes my work-up and consideration for dangerous causes of CP can be done right at the bedside with a good history and exam. I can listen for pneumonia or pneumothorax. I will check vitals signs (as you will see) and look at an ECG and labs if necessary.
With anxious patients, I have found it helpful to list out diagnoses that I know are NOT present in terms that they can understand, such as…
”I do not see signs of a heart attack on your EKG or lab work-up and you don’t have any risk factor or signs for blood clots in your lungs. Your symptoms and exam don’t sound like a collapsed lung or pneumonia. Are there other things that you might be worried about that I could address?”
Many patients and family members appreciate a speech like that so consider adding it to your “standard” work-up if you don’t already. As for routine documentation, because this conversation varies so much from patient to patient, I don’t include it in my CP template.
On to the vitals and exam!!